The growth of digital healthcare has given rise to new definitions for provider-patient interactions. Among the commonly used terms, we often hear of EMR (Electronic Medical Records), EHR (Electronic Health Records) and PHR (Personal Health Records). Most often these terms are used interchangeably to refer to online health records. However, they are known by different names due to being defined based on the degree of ownership and accessibility of the health data.
Electronic Medical Records (EMR)
EMR refers to health records that are solely owned by a particular health organization, be it a hospital, clinic or individual doctor. It consists of information that is collated by the physician for their patients’ diagnosis and treatment. It is primarily recorded for internal use and does not travel outside the medical practice.
Benefits of EMR
- It does away with paper records
- Allows providers to continuously track their patients’ health data over time
- It helps identify patients who are due for screenings or follow-ups
However, with EMR, patients do not have access to their health records and if needed, they will have to obtain a printed version of the same to share with other health providers. It only offers health providers a partial record of the patient’s health, limited to the information that is collected from that hospital, clinic or doctor’s office.
Electronic Health Records (EHR)
EHR is similar to EMR but goes beyond just clinical data gathered in one doctor’s office. EHR represents a collection of health data from all clinicians involved in a patient’s care – right from physicians and specialists to clinicians from laboratories and diagnostic centres. This comprehensive health record can also be shared with other healthcare providers as it is created by the provider but made to be more patient-centric, making it more powerful and useful for diagnosis and treatment compared to EMR.

Benefits of EHR
- It can be shared with multiple health providers for collaborative patient care
- Patients are more actively involved in their care as they can view their health records and are aware of their diagnoses and treatments
- It enables continuous health monitoring by providers
- Continuity of care is ensured among care providers as patient health information is readily accessible
- Unlike EMR, these records are truly paperless
Personal Health Records (PHR)
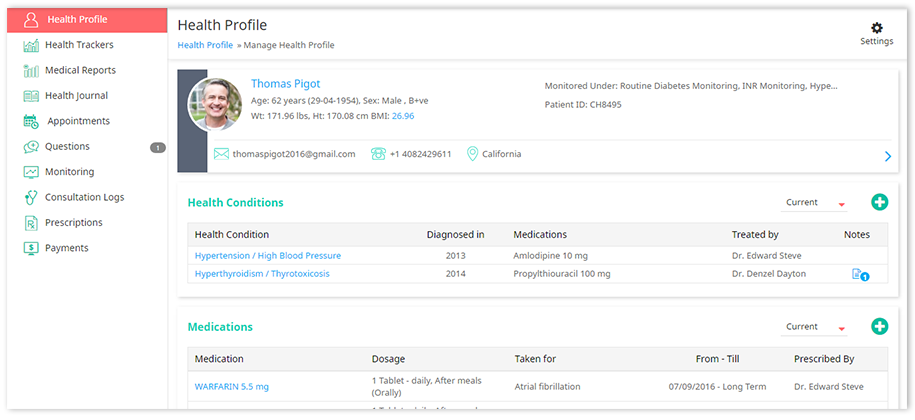
As the name suggests, PHR is managed by the patients themselves. This allows them to maintain a log of their health- allergies, medications, treatments, health conditions, family medical history and more. PHR is set up either by health providers or by patients themselves, for patient engagement or personal use. Patients can actively participate in their care and are more empowered to make decisions about their health as they have all the vital information available to them. Like an EHR system, they can also choose to share this information with their doctors when needed. Information in PHR often includes a combination of clinical information from doctor visits, medical and lab reports and data they may be monitoring themselves from home monitoring devices or wearable activity trackers.
Benefits of PHR
- Empowers patients to be actively involved, thereby improving adherence and health outcomes
- Health data in a PHR can be shared with various providers for second opinions and follow-up care
- Provides doctors with a comprehensive understanding of their patient’s health, including details about familial medical history and social factors impacting their patient’s health
- Allows for effective home care and remote monitoring as patients can actively provide updates to their care providers
- Allows all the patient’s doctors to work together as a team, minimizing health complications
The information in a PHR can be thought of as a combination of data from an EHR, together with patient-generated health data. This is more closely tied to meaningful use as it is powered by the patients, for their own care.
What is the future of electronic health data?
Most health providers have relied heavily on EMR systems in their hospitals, offices or clinics for storing and managing patient data. But given the obvious gaps with this system of health record management, there has been a need to update and improve how health data is shared and utilized in healthcare delivery.
In order to make it mutually beneficial to patients and providers, many government organizations have insisted that health providers use the more robust EHR system. This is mainly because it is more patient-friendly and transparent and attempts to address some of the gaps of the EMR system. Secondly, it also limits errors in decision-making as it gives providers a better understanding of their patient’s medical history and health conditions.
On the other hand, Personal Health Records has gone one step further to ensure meaningful use of patient health data. It offers all the benefits of EHR, with the added benefit of more patient involvement as the health data is managed and owned by them. PHR provides doctors insight into patient health outside the purview of the hospital or clinic, allowing for better understanding of patient health, which improves health outcomes.
With the Virtual PracticeTM, the PHR ties into most of its features to enable patient engagement and improve collaborative care. For instance,
- Patient Portals can be used to get patients to add in data to their PHR online
- The ContinuousCare mobile app for patients allows them to store, view and update their health records on-the-go
- The Virtual PracticeTM includes health trackers which allow providers to capture health parameters continuously and not just as one-time readings, providing greater insight into patient progress
- Getting patients to participate in their health opens up the possibility of remote monitoring, which in turn unlocks new revenue opportunities for health providers
- The ContinuousCare patient app is compatible with Apple HealthKit and Google Fit which therefore makes it possible for providers to get data from devices that are linked to both these platforms. This includes various fitness, diet and exercise apps as well as home health monitoring apps like iHealth devices that measure blood glucose values.
The Virtual PracticeTM is a patient engagement, practice management and patient management platform for health providers. It offers providers the capability to improve their online presences through its patient portal, which includes telemedicine services like video consultations, revenue management capabilities and patient data management through Personal Health Records. More about the services of the Virtual PracticeTM.