After logging the patient encounter under the Encounter Log, you can use the AI Scribe to draft a structured, professionally formatted clinical document.
Drafting a New Document with AI Scribe:
To create a new document, Start by selecting the appropriate template, such as a SOAP Note or Patient Visit Summary, etc.
Creating a Document using AI Scribe
While a default template is shown for ease of use, the Provider can search for any other templates in your Virtual Practice, including those in your Template Library or built-in templates.
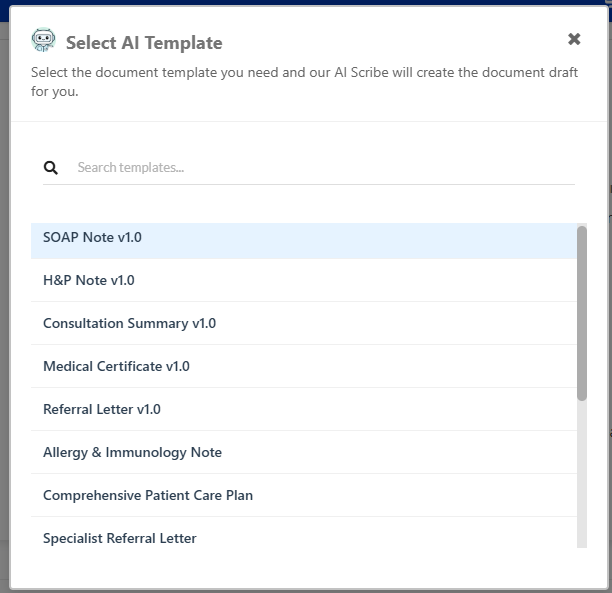
Selecting an AI Template
The AI Scribe will draft an organized clinical note that follows proper medical documentation standards and includes all the essential elements for your chosen document type.
The AI Scribe-generated document organizes information logically from multiple sources: information from the encounter transcript and any notes that you might have manually added during the consultation. It also incorporates relevant context from the patient’s existing health record, including current health conditions and medications, known allergies, social history, and family medical history.
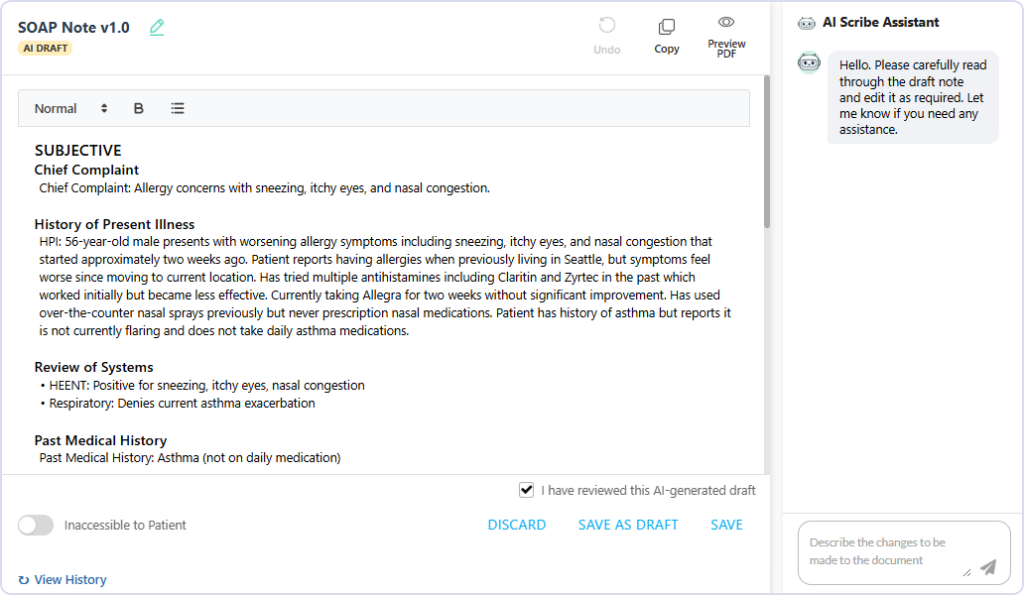
Generated Consultation Document using AI Scribe
While AI Scribe never replaces clinical judgment, it can provide helpful organizational structure for clinical reasoning and treatment planning. Based on documented symptoms, examination findings, and clinical context, the system can suggest relevant diagnostic considerations or treatment approaches for your review.
The Provider can Discard a document before saving if required. Discarding will permanently remove the created template document.
Reviewing, Editing, and Finalizing the Document
Once AI Scribe generates the initial document, providers must carefully review and edit the content to ensure clinical accuracy and completeness. Alternatively, the Provider can also choose to discard the document draft or save it as a Draft to work on later. The document editor supports formatting and undo options.
This review process can be conducted through traditional manual editing or by providing AI Scribe with specific instructions for modifications, such as adding clinical insights, refining diagnoses, or restructuring sections.
The provider retains full control and responsibility for the final document content and clinical decisions. It is not possible to save a document as final without confirmation or review and correctness.
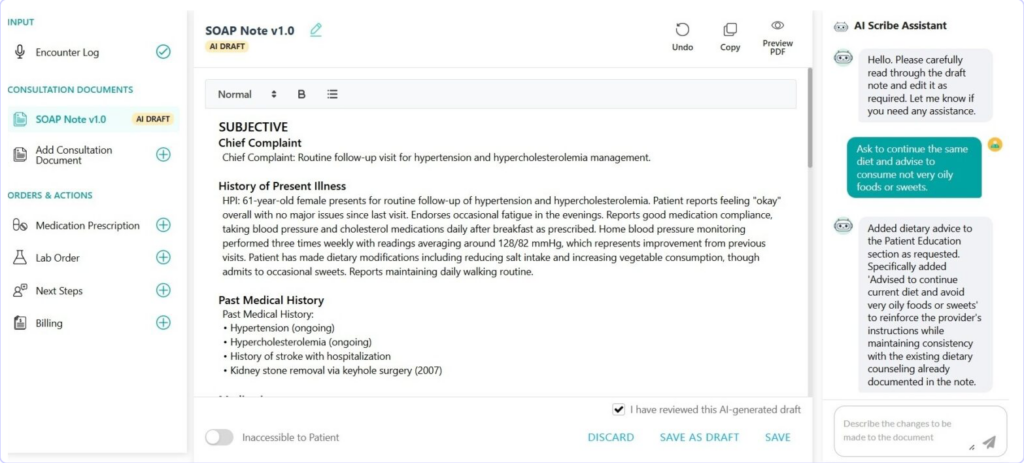
Provider Editing the Generated Consultation Document by chatting with the AI Scribe Assistant
Once a document is saved, the Provider’s signature (if the signature image file is configured in the provider’s account) will be included in the final document. If the Virtual Practice requires its providers to eSign each document, that option will be displayed at the bottom of the document.
Setting Patient Accessibility
Providers can decide whether a document should be accessible to the patient involved in the consultation. If making it accessible, the document will be securely accessible to the patient through the patient portal or patient app. Patients can be optionally notified when a document is available in their account. The accessibility of documents follows the default setting in the document template e.g. the Patient Consultation Summary document is accessible by default. Providers can however override this setting per document that they create.
Creating More Consultation Documents for the Consultation
It is important to note that you can create more than Consultation Document for a patient consultation, for example you can create SOAP Note for your records and also a Patient Visit Summary for the patient. For patients requiring referral to another healthcare provider you can create a Referral Letter or choose to issue a Medical Certificate for a patient needing that for their place of work or study.
Viewing, Downloading, and Printing PDF Version
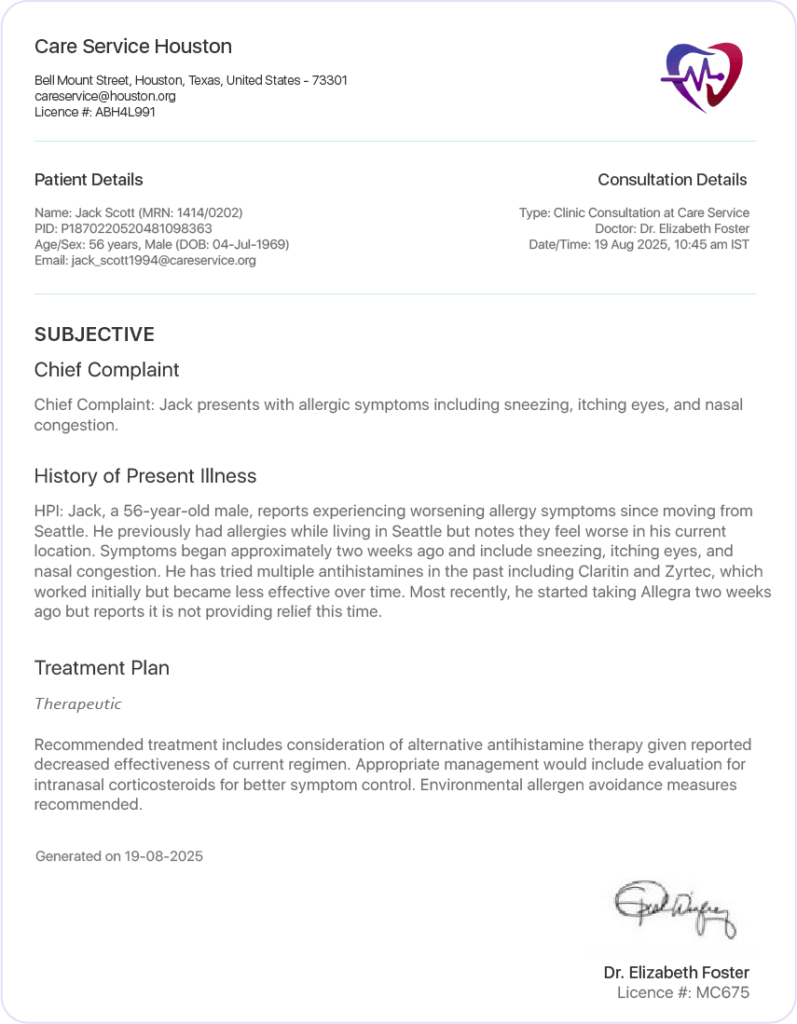
PDF Preview of Consultation Document
All Consultation Documents have their content integrated into the standard PDF Document format supported in the Virtual Practice. The document header includes the configured logo of the Virtual Practice and details of the relevant Practice Location.
It also includes a summary section containing relevant details of the Patient and Consultation. The main document content is displayed below these sections, followed by the Provider’s signature, including the provider name, qualifications, and licence.
Optionally, the document can also include a standard disclaimer content section to display any content that the customer chooses to display there. This content will apply consistently across all Consultation Documents in the Virtual Practice.
Cancelling a Consultation Document
A Provider can choose to Cancel a saved Consultation Document. It will be retained in the application interface for the provider in the ‘Cancelled’ state. If the document had been shared with the patient, it would no longer be available to the patient to access. The patient will receive a notification that a document has been cancelled.
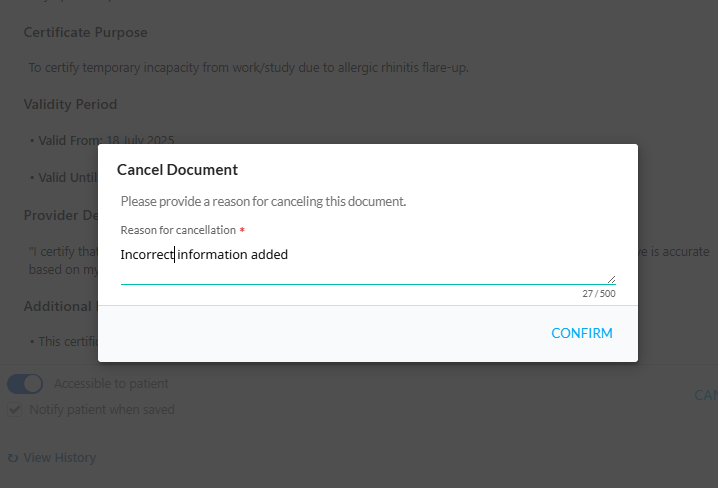
Cancel Consultation Document
Explore comprehensive guides for each aspect of the Consultation feature:
